Shoulder Pain: Raising the level of diagnostic certainty about SLAP lesions
Many shoulder-pain patients present with symptoms suggestive of a superior labrum anterior and posterior (SLAP) lesion. These include pain with specific shoulder positions, pain during overhead activities such as tennis or throwing sports, or impaired shoulder strength. A range of patients with varying ages and activity profiles can experience these symptoms. As a result of the clinical frequency of SLAP-like symptoms, approaches to SLAP lesion management currently generate much discussion, including the possibility of surgical overtreatment.Best Slap Tear Shoulder Surgery can decrease the pain from the shoulders biceps tendon inserts into the superior labrum
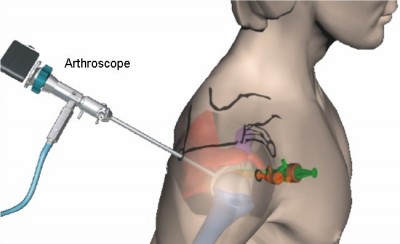
The rise of magnetic resonance imaging (MRI) with gadolinium dye helped bring more attention to SLAP lesions. These advances made it possible to visualize SLAP lesions preoperatively.
Identifying causal factors
To minimize the risk of overtreatment, renewed effort should be directed toward meticulous execution of the initial clinical exam and correct diagnosis. "The greatest need right now in the treatment of SLAP lesions is to raise the level of diagnostic certainty that a SLAP lesion is responsible for patients' symptoms, or the substantial contributing factor, and not just a coincidental finding.
The challenge rests on distinguishing a painful SLAP lesion from an anatomic variation. Degenerative lesions and age-related wear, along with fraying or splitting of the labrum, have to be ruled out. They are not the source of the pain — and, therefore, likely will not benefit from a repair.
The basic question we address in our research on improving diagnosis is, how do you determine a SLAP lesion is causing pain, and how do you know a patient with pain has a SLAP lesion?
Sports Medicine
SLAP lesion mimics
As imaging continues to improve and more people undergo MRI studies, physicians are finding that a significant percentage of people within the general population have labral changes that do not cause symptoms or need repair. In particular, there are age-related changes that can cause degenerative splits and tears in the labrum. While they may not be symptomatic, visually they can mimic a SLAP lesion. When these appear in MRI studies, misleading assumptions may be made between the images and the patient symptoms.
Key clinical skills that a practicing orthopedic surgeon needs are familiarity assessing a patient with shoulder pain and a means for determining the presence or absence of a causal relationship among anatomic pathology, symptoms and functional impairment. Complicating the task of making the correct SLAP lesion diagnosis is the fact that SLAP lesions can occur as part of other pathologies, such as partial thickness rotator cuff tears or biceps tears.
Risk factors
Males in their teens or 20s, a group that tends to be physically active, are at highest risk of shoulder dislocation.
Dynamic labral shear test
To raise the level of diagnostic certainty when a SLAP lesion is suspected, Dr. O'Driscoll has developed a clinical maneuver, the dynamic labral shear test (DLST). The DLST reproduces the shearing mechanism that can cause a SLAP tear. Easy to perform in the exam room, the DLST yields reliable results that isolate a SLAP lesion's causal role in symptoms and impaired function.
To prepare for the DLST, the patient is supine and relaxes the affected arm off the side of the examining table. The shoulder is close to the edge of the bed so that the examining table mattress supports the scapula, but the humerus is free.
Performing the DLST
For the right shoulder, with the arm at the side, the examiner flexes the right elbow 90 degrees and grasps the olecranon and distal humerus with his or her left hand. This hand is used to maintain 90 degrees of elbow flexion, passively rotate the shoulder externally to its natural limit with the force of gravity alone pulling down on the forearm, drop the elbow back into its natural limit of horizontal abduction (toward the floor), and passively elevate the shoulder while maintaining both the horizontal abduction and the external rotation at their natural limits under gravitational force alone.
During elevation of the shoulder, the magnitude of horizontal abduction will vary and must be permitted to do so without constraint. Similarly, the degree of external rotation will also vary throughout the arc of elevation and must be unconstrained. While the shoulder is being elevated in the manner just described, the examiner's right hand is kept on the acromion to stabilize the scapula and to detect any palpable click transmitted through the bony structures. The click will usually be felt by the left hand on the olecranon, as well as the distal humerus. After full overhead elevation, the entire motion is reversed and the arm is brought down to the side while the natural limit of shoulder external rotation and horizontal abduction is maintained.
Interpreting results
Interpreting the results requires skill and experience with the maneuver and its physiologic effects.
About Doctor:
Dr.KHALEELULLAH is a renowned gold medal award-winning Orthopaedician in Hyderabad. He has got extensive experience of more than 15 years and positioned himself as the best orthopedic surgeon in Telangana and Andhra Pradesh. He worked for nearly 8 years in the prestigious Nizams Institute of Medical Sciences(NIMS), Hyderabad where he acquired vast skills and knowledge about managing complicated orthopedic problems. He proved himself as the right Ortho Surgeon with MCH specialization with his deep interest in the area of joint reconstruction surgeries.

